The New NetHealth Library
Patty Scheets, Vice President of Quality and Compliance
After years of waiting and months and months of much work behind the scenes, we were finally able to roll out the new content for the skilled nursing (SNF) electronic medical record (EMR), NetHealth™. As I write this, our users are experiencing the highs and lows of something new. Some are finding a streamlined process with helpful tips and tricks. Others are feeling less efficient as they try to find where things are. And others, still, are simply frustrated – what was wrong with the old content?
None of these responses is surprising, and they all prompt me to share a bit about the philosophy behind the changes…the “why,” if you will.
Very early in my career, our documentation platform was a blank piece of paper and an outline of critical elements to be included. My first supervisor read every one of my handwritten notes, and if she could not “see” the patient, understand my hypothesis for the nature of their movement problem, identify my prognosis for recovery of function, and recognize a well-defined plan, she gave it back to me to try again.
While our documentation process has evolved in so many ways since the first days of my career, the fundamental principle, that the documentation platform we use as clinicians shapes who we are as clinicians, has not changed. In the preface to the third edition of their book, Documentation for Rehabilitation: A Guide to Clinical Decision Making in Physical Therapy,[1] authors Quinn and Gordon state, “. . .not only is the logic of clinical reasoning reflected in documentation, but documentation itself shapes the process of clinical reasoning.” In the foreward of the same text,1 Derick Wade, a well-known and respected researcher and Professor of Neurological Rehabilitation at Oxford, begins with the following: “Good documentation is associated with good decisions. . . .if good documentation is provided, then it helps in the analysis of a situation because it can impose a framework upon the user to facilitate understanding.”
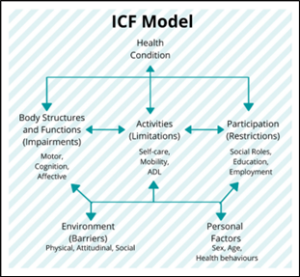
With these foundational concepts in mind, when designing the new content, the challenge before us was to provide a systematic approach to clinical decision-making that would be effective and efficient and within the constraints of an established EMR. To achieve this systematic approach, we relied heavily on three rehabilitation related frameworks. The first of these, the International Classification of Functioning Disability & Health (ICF)[2],[3] is depicted in Figure 1. This framework was developed by the World Health Organization and is commonly used to describe the domains of factors or characteristics of individuals that can have positive or negative effects on their function and health. The language of the ICF domains is used throughout the new library with minor adjustments in occupational therapy to align with the American Occupational Therapy Association’s integration of these concepts into their practice framework.[1]
Figure 1. The International Classification of Functioning Disability and Health. The domains of this framework are integrated into the new library. See the glossary for further definitions.
The second “big idea” integrated into the new library is the concept of different rehabilitation pathways4,[1],[2] which is shown in Figure 2. Thinking through our rehabilitation interventions in this fashion pushes us to go deeper into understanding the nature of a patient’s problem and the likelihood of the related impairments in body structure and function improving. When we are indiscriminate in how we select remediation versus compensatory strategies, we can waste time, inadvertently add to a person’s disability, or fail to fully integrate new strategies into context. The goal of the decision-making support around this concept in the new library is to guide us toward the critical questions and high value solutions.
The final concept that has been fully integrated into the library as a means of understanding how patients may be changing is thinking about the rehabilitation process as an opportunity to assist individuals in building skill.1 According to Quinn and Gordon,1 skill is the ability to achieve a desired outcome with consistency, flexibility, and efficiency where:
- Consistency = successfully performing over multiple trials or days
- Flexibility = performing under a variety of environmental conditions
- Efficiency = performing within a certain level of energy expenditure.
Figure 2. Rehabilitation pathways defined. Choosing the correct pathway has important implications for the patient’s outcome and the value of care we provide.

The language of building skill is a nice way to encapsulate what we do that extends beyond improving the level of physical assistance a person needs to complete an activity. It gives us the vocabulary to describe the important performance characteristics we can measure to determine if the patient is moving forward or failing to progress. It gives us ideas for important ways in which we can challenge patients to maximize their performance. It reflects the specificity and complexity of the work we do.
And, speaking of specificity and complexity, I want to acknowledge the work of Kim Gabourel and Lori Waller who embedded themselves in the hidden parts of NetHealth™ to achieve “the why” within the constraints of the system. The process has been overwhelming, challenging, tedious, time consuming, and all consuming, and we are extraordinarily fortunate to have two individuals whose personal skills and interests aligned so well with what was needed. Many, many thanks to Kim and Lori!
Finally, see a companion article describing the process for submitting feedback or suggestions. You may find additional supporting materials on the Springboard here (login required).
_______________
[1] Quinn L and Gordon J. Chapter 7: Documenting activities. In: Documentation for Rehabilitation: a guide to clinical decision making. 3rd ed. Saunders Elsevier, 2016:vii-xi, 107-120.
[2] Ustün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The International Classification of Functioning, Disability and Health: a new tool for understanding disability and health. Disability and Rehabilitation. 2003;25(11-12):565-571.
[3] Bruyère SM, Van Looy SA, Peterson DB. The International Classification of Functioning, Disability and Health: Contemporary Literature Overview. Rehabilitation Psychology. 2005;50(2):113–121.
[4] American Occupational Therapy Association (AOTA). Occupational Therapy Practice Framework Domain & Process 4th ed). Am J Occupational Ther. 2020;74(Suppl 2),7412410010. https://doi.org/10.5014/ajot.2020.74S2001.
[5] Levin MF, Kleim JA, Wolf SL. What do motor “recovery” and “compensation” mean in patients following stroke. Neurorehabil and Neural Rep. 2009;23(4):313-319.
[6] Maier M, Ballester BR, Verschure PFMJ. Principles of neurorehabilitation after stroke based on motor learning and brain plasticity mechanisms. Front Syst Neurosci. 2019;13:74.