The MDS Changed on October 1 – What Do I Need to Know?
By Patty Scheets, Vice President, Quality and Compliance
Note: a PDF download of this content is available at the end of this article.
On October 1, the Minimum Data Set (MDS) used for clinical assessment and related reimbursement in skilled nursing was updated to version 1.18.11. The purpose of this article is to summarize the big changes so that each of us may be more prepared for our role in the interdisciplinary team.
Global changes incorporated into this version of the MDS include gender-neutral language, updates in wording and examples to clarify and enhance understanding, changes to the quality improvement and evaluation system, and guidance for the use of patient proxy when gathering data. In the subsequent section, I’ll highlight some of the changes to the MDS items as well as what we’ve done with the next version of the NetHealth library to support MDS data collection.
Social Determinants of Health (SDOH)
These are the conditions in which people live, work, learn, and play and have been shown to affect a wide range of health risks and outcomes. These data help us understand the impact of these factors on outcome, document and track health disparities, and allow for comparison of these factors across post-acute settings. In the language of the International Classification of Functioning Disability & Health (ICF), these are often part of personal and environmental factors. In Section A, there are now more detailed items to describe race and ethnicity. An added item (A1250) relates to how a person’s access to transportation impacts their ability to receive medical and non-medical services. In section B (B1300), there is a question about health literacy. Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. In this item, the patient is asked to respond to how often they need help to understand health information. In section D (D0700), patients are asked about how often they feel lonely or isolated. There are specific coding rules MDS and nursing staff will use to score these items correctly if the patient is unable to respond.
Changes you’ll see in our documentation related to these items are:
- The addition of transportation issues as an environmental factor in each of the evaluation and other documents.
- There is an opportunity to comment on your perception of the patient’s health literacy in the background information of the evaluation documents.
- There is an opportunity to comment on the level of social isolation the patient may be experiencing in the background information of the evaluation documents.
Mental Status
There were no changes to the Brief Interview for Mental Status (BIMS) items, but there are revisions to the steps for assessment. These include conducting the interview in a private setting if possible and ensuring that the person conducting the interview can articulate the items clearly. If a patient chooses not to answer, accept their refusal and move on to the next question. Refusals are coded on the MDS as incorrect/no answer or could not recall. If a patient’s primary method of communication is in writing, the BIMS may be completed in writing. The interviewer may also stop the BIMS if, after completing “day of the week,” all responses have been nonsensical, or the patient has not responded.
These updated instructions are added to the hover in the BIMS section of the speech evaluation document.
Functional Status
Best practice has always been to complete the MDS using an interdisciplinary process which should include information about patient performance from all staff interacting with the patient. In this version of the MDS, for patients in a Medicare Part A stay, there is an increased emphasis on conducting the admission functional assessment prior to the benefit of services. This emphasis makes it more urgent for us to score section GG items without providing physical, verbal, or set-up assistance with each task.
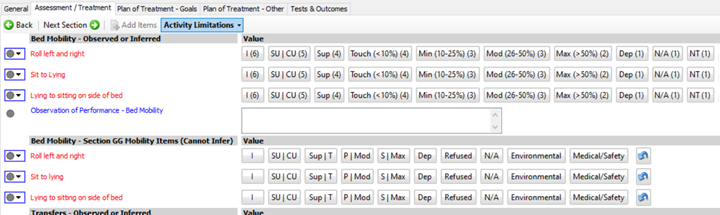
We recognize that information about activity limitations/occupations is heavily sought by payers, MDS coordinators, directors of nursing, and other rehab staff. In response to feedback from all of these sources, in our existing library version, we expanded the section GG scale by splitting the Supervision/Touching level into 2 levels (SBA and CGA) and the Partial/Moderate assistance into Minimal and Moderate assistance. When we did this, we were no longer able to complete the section GG form by copying from document.
In the newest version of the library, we have done 2 new things: 1) We adjusted the names of the levels of our expanded scale to make it more clear which levels were split from Supervision/Touching of the GG scale. These new buttons now read Sup and Touch rather than SBA and CGA. 2) We integrated the section GG items within the activity limitations tab. As you can see from the figure below, there are a group of items to score with the expanded scale, then the same items using the GG scale. By positioning the items close together, we are hoping to decrease the cognitive burden of scoring section GG. Now, when you go to the GG form, you may select copy from document, and the form will populate with the scores you entered on the GG items.
There has been clarification in the supervision/touching and dependent codes. If a patient requires only verbal cueing to complete an activity, score as supervision/touching. If a patient requires a second person to complete an activity code the activity as dependent regardless of the amount of assistance they provided and even if the assistance just for managing equipment.
This guidance was added to the hover in the appropriate sections.
There are a couple of changes to bed mobility tasks.
- If a patient does not sleep in a bed, assess bed mobility tasks using the alternative furniture the patient uses for sleeping.
- Lying to sitting on the side of the bed now does not require the patient to end with their feet flat on the floor.
- Car transfer includes just the ability to get in/out of the car on the passenger side. It does not include opening/closing the door or fastening the seat belt.
In previous versions of the MDS there was a section G and a section GG. In this version, items in section G have been moved to section GG. These include functional limitation in ROM, mobility devices used, personal hygiene, and bathing (tub/shower transfer). None of these new GG items is required.
- Information about ROM limitations is documented in our evaluation documents under impairments in body structure and function (PT) or client factors (OT).
- Mobility devices are identified in the background information of the evaluation documents.
- We have added personal hygiene and shower/tub transfers to the OT documents.
Pain Assessment
There is a new MDS item, J0510, which replaces previous pain related items and measures the frequency with which the patient has pain that interferes with their sleep. There is also a new item (J0520) which asks, “Over the past 5 days, how often have you limited your participation in rehabilitation therapy session due to pain.
- In the evaluation documents for OT and PT, there is a required question about whether the patient has pain that interferes with functional activity or sleep.
- In OT, this is under Client Factors – Musculoskeletal/Pain
- In PT, this is under Integumentary/Pain
- For all disciplines’ treatment notes, under the subjective section, there is a place to report pain at rest and provide additional detail.
- In the PT and OT treatment notes:
- For each treatment element provided, clinician role, there is a place to indicate what strategies the clinician used to help manage pain.
- There is a place in patient response, exertional intolerance, to indicate pain level and location during or after the session.
- Bringing this level of information to the IDT, will assist the community in obtaining an accurate representation of how pain in impacting the patient during their stay.
Other Helpful Tips
With the change to PDPM, there was an increased emphasis on skilled nursing care as compared to the previous RUGs system. Because the transition to PDPM was followed so closely by the pandemic, many of us are still adapting to this new structure. We may make observations during our sessions which may be triggers for nursing assessment, monitoring, teaching, and training.
In the newest version of the library, we’ve incorporated some clinical observations. Look for them under patient response, exertional intolerance or incorporate your observations in comments related to when/where you observed them.
- SOB while lying flat – may be associated with pursed lip breathing or persistent cough – may be associated with a nursing special care high category
- SOB with oxygen – may be associated with a nursing special care low category
- Changes in oxygen saturation associated with pneumonia – may be associated with a nursing clinically complex category
Support for these nursing categories must be found in the nursing documentation, but sharing our observations with the interdisciplinary team may assist the community in recording a more accurate clinical picture of the patient.
For More Information
If you’d like to learn more, you may review the slides from our consultant, Ellen Strunk, Rehab Resources and Consulting, they are available to download below. You may also find the source document here: Minimum Data Set 3.0 Resident Assessment Instrument User’s Manual v1.18.11 (cms.gov).