Clinical Outcome Measurement: Why Does it Matter?
Patty Scheets, Vice President of Quality and Compliance
During 2025, we’ve been rebuilding our clinical dashboards which has made it possible to visualize how we are doing collecting clinical outcome data and, subsequently, how we are doing with our patient outcomes. In this edition of the Insider, I want to focus on three areas related to clinical outcomes:
- An update on our adherence to collecting the Infinity-specific outcomes
- A change in the rules for testing Section GG
- The link between our clinical outcomes and the CMS Quality measures, specifically Expected Discharge Function Score and Expected Discharge Mobility and Self-Care Scores
Adherence to Outcome Measurement
Performance improvement best practices recommend that when embarking on a new or renewed clinical practice, you will have better success if you focus your attention. In this spirit, we opted to focus our attention on adherence to collecting the physical therapy measures, the Short Physical Performance Battery and the 6-Minute Walk Test. Each week, we’ve been reporting the percentage of patients admitted for a skilled Medicare A (or similar) stay for whom we have collected these measures at evaluation and discharge. A chart illustrating adherence to these measures is shown below.
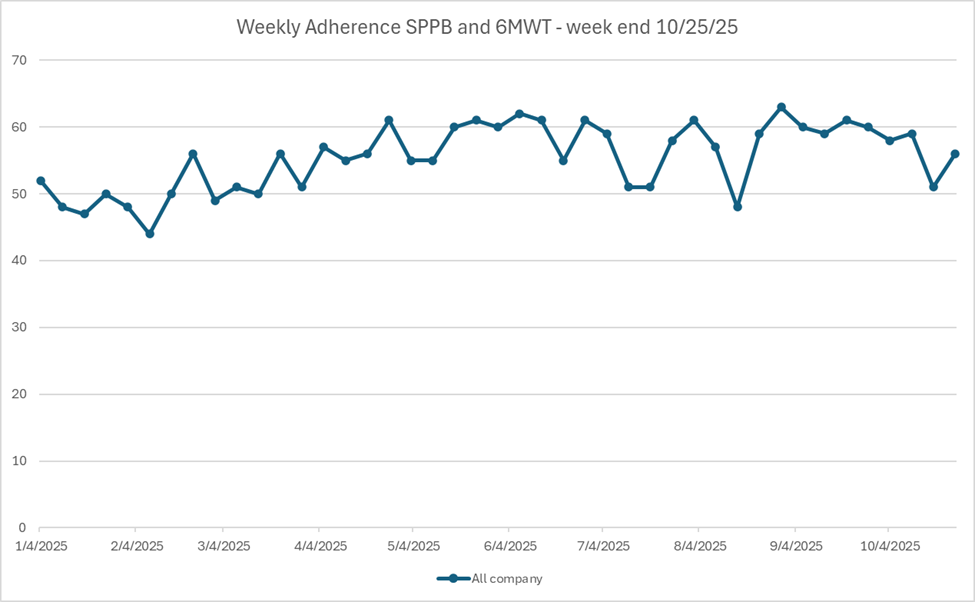
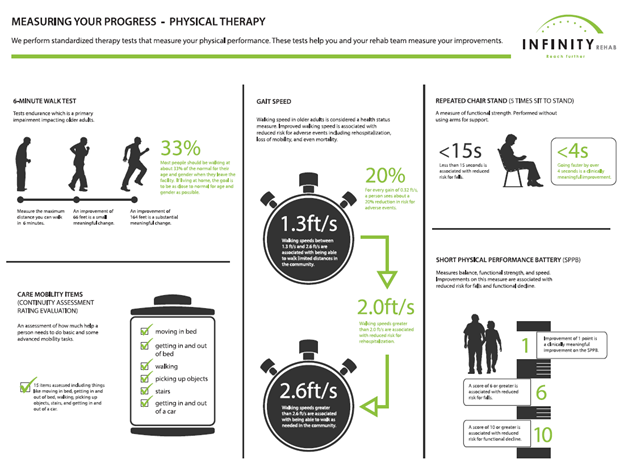
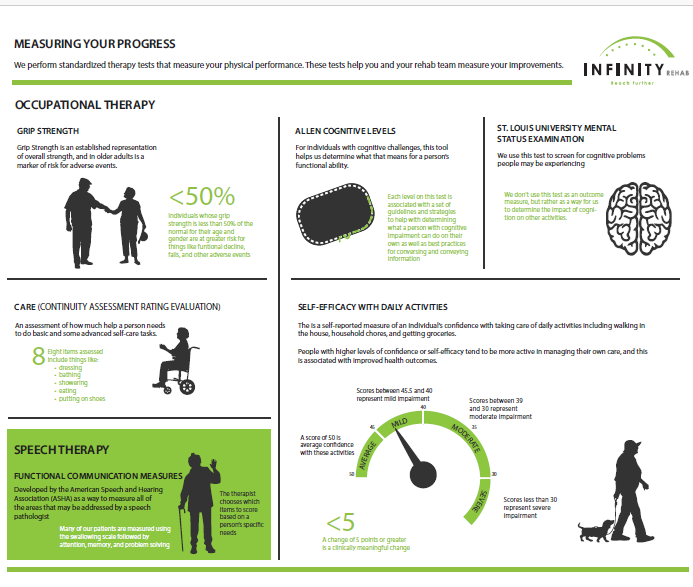
You can see that we have been above the 50% mark for months and that in recent weeks we’ve been hovering close to 60%. To get to these results, locations have been implementing systems and best practices for collecting and tracking data, including strategies for PRN clinicians to know how and when to collect data, and being prepared with discharge values should there be an unexpected discharge. (If you are struggling with data collection either personally or within your community, feel free to contact me at plscheets@infinityrehab.com so we can problem-solve together.) The most critical step to ensure data collection, however, is to use the results of the measures to guide and direct clinical decision-making. If you need a refresher on what these tests measure and more about their meaning, take a look at the education tools pasted below. Pro tip: request poster versions of the graphics below for your community by emailing our marketing department.
Updated Rules for Section GG
In October of each year, CMS updates the Resident Assessment Instrument (RAI) Manual which governs the rules for completing the MDS. This year, there was a subtle but important change to the rules for completing section GG. I’ve copied the text below:
Assessment of the GG self-care and mobility items is based on the resident’s ability to complete the activity with or without assistance and/or a device. This is true regardless of whether or not the activity is being/will be routinely performed (e.g., walking might be assessed for a resident who did/does/will use a wheelchair as their primary mode of mobility, stair activities might be assessed for a resident not routinely accessing stairs).[1]
I just want to say, I love this change!! Too often we have failed to observe complex activities (especially stairs!) because patients do not routinely encounter them. But stair climbing is such an important functional marker for older adults.[2] It requires balance, strength, and endurance at a level that puts a healthy challenge in front of our patients. Stair negotiation time is a predictor of functional decline.[3] Ascending and descending stairs as an intervention meets all the criteria for the type of exercise (balance + functional + resistance) which can reduce the rate of falls by approximately 34%.[4] Focusing on stair climbing and other challenging tasks is also consistent with the leap frog principle of rehabilitation in which an early focus on more challenging tasks leads to a better outcome both in rate of improvement and discharge performance.[5]
Quality Measures – Discharge Function, Mobility, and Self-Care Scores
The Discharge Function Score (DFS) is a cross-setting functional outcome measure used in the SNF Quality Reporting Program and a part of the 5-Star Program.[1] This measure shines a light on the role of functional status and a SNFs quality of care. In the technical report describing the measure CMS highlights the importance of the type of therapy provided as a factor that influences this important measure of quality.6 The DFS determines how successful a SNF is at achieving an expected level of functional ability at discharge. The items in the measure are applicable across all settings (SNF, IRF, LTAC, HH) and include: eating, oral hygiene, toileting hygiene, rolling left and right, lying to sitting, sit to stand, chair/bed transfer, toilet transfer, walk 10 feet, walk 50 feet with 2 turns, wheel 50 feet with 2 turns. The DFS calculates the percent of Part A SNF residents who achieve a risk-adjusted expected function score at discharge. The coefficients used in the risk adjustment model include admission function, age, and resident clinical characteristics. If an item is left blank on the MDS or not scored using the level of assistance scale (values 1-6), the item score is estimated through a statistical process. The Expected Discharge Mobility and Discharge Self-Care scores are similar to the DFS but include all the items in the respective set. These measures are also a part of the SNF Quality Reporting Program.
How can we help our communities be successful with these measures? First of all, look at the type of therapy we are providing. Are we providing high-intensity aerobic and resistance training? Are we using our patient self-management strategies to engage the patient? Are we initiating early caregiver training for patients who are not as responsive to care? Have we tailored our plan to meet the patient’s cognitive level and to what matters most to them? Let’s live into our mission to deliver the best of science with the art of caring and help all our communities and patients do better than expected when they leave our care!
__________________________________
[1] https://www.cms.gov/files/document/final-mds-3-0-rai-manual-v1-20-1-october-2025.pdf
[2] Startzell JK, Owens DA, Mulfinger LM, Cavanagh PR. Stair negotiation in older people: a review. J Am Geriatr Soc. 2000;48:567–580. [3] Oh-Park M, Wang C, Verghese J. Stair negotiation time in community-dwelling older adults: normative values and association with functional decline. Arch Phys Med Rehabil. 2011 Dec;92(12):2006-11. [4] Sherrington C, Fairhall N, Wallbank G, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb S. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med. 2020 Aug;54(15):885-891. [5] Hord SD, DeJong G, Smout RJ, Gassaway J, James R, and Conroy B. Stroke rehabilitation patients, practice, and outcomes: is earlier and more aggressive therapy better? Arch Phys Med Rehabil. 2005;86(2):S101-S114. [6] https://www.cms.gov/files/document/snf-discharge-function-score-technical-report-february-2023.pdf-0